< Back to Sanius content
Capturing the Patient Experience During a Vaso-occlusive Pain Crisis | What Can We Learn from First-hand Insights?
If you ask a patient with sickle cell disease (SCD) to describe exactly what a pain crisis feels like, among the common keywords is often a simple statement that it is something that cannot truly be captured in words. Beyond the physical pain and impacts in terms of progressive organ damage is a devastating toll on patients’ mental health and daily activities, and oftentimes, the only way forward is managing the pain and waiting for the episode to pass.
With new treatments that seek to make patients’ day-to-day experiences and quality of life better still battling roadblocks to wider access, a critical component of improving patient lives is working towards a route to the prevention of VOCs. To do this, understanding the early signs and triggers of a crisis and what can help to stop them in their tracks is critical.
This forms a core part of Sanius’s ongoing work, driven by an ecosystem of unified retrospective and prospective medical record, genomic, wearable, and patient-reported outcomes data. Collected continuously and objectively, this information builds a full picture of patients’ physiological health and quality of life at a longitudinal level, providing patients and their clinical teams with a new understanding of their condition each day.
Recently, we have also begun to explore the first-hand feedback from patients, focused on what they experienced during their most recent VOC, how they treated it, and what happened in the week leading up to it. Our hope is that, from this real-world insight, we can begin to build the foundation for early detection, intervention, and prevention.
Characterising the VOC.
Patients were invited to share their experiences during the VOC through a digital online survey. 7% of patients described still being in the midst of a crisis, with the remaining patients reporting a mean duration of 7 days. Most of these VOCs were first experienced at home, before more than half of the patients were forced to seek clinical support in hospital as their severity progressed. While several patients reported multiple regions in which they felt their VOC pain, chest pain was the most common, followed closely by back pain. Additionally, overall “joint” pain as well as more specific knee, hip, ankle, wrist, shoulder, and elbow pains appeared frequently in patient responses.

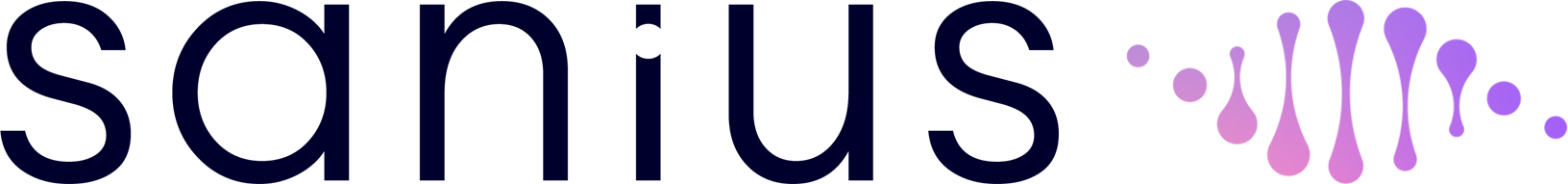
When asked to describe what the VOC felt like, “stabbing” pains were the most frequently reported (35%), with many phrases linked to a heightening and falling pattern of pain – sometimes described to be like a heartbeat. 12% of patients experienced breathing difficulties or shortness of breath during the VOC, with a further 7% describing tightness or pinching sensations and 5% reporting the feeling of a heavy load on their chest. Beyond these more physical descriptors were ones linked to the psychological impact of the VOCs, including “excruciating” and “unbearable”.
Signs and Triggers of a VOC.
A critical component of the survey was further advancing what is known about the days prior to a VOC. While no two patients’ experiences are ever identical, a number of key similarities were identified across the cohort. Indeed, pain and aches were expected and commonly reported presences in the 7 days before the VOC, alongside feelings of tiredness, fatigue, overwork, and physical exertion. Despite this, a notable proportion of patients reported no warning signs, stressing the need for new ways to identify the silent markers of a VOC when tackling the challenge of proactive intervention.
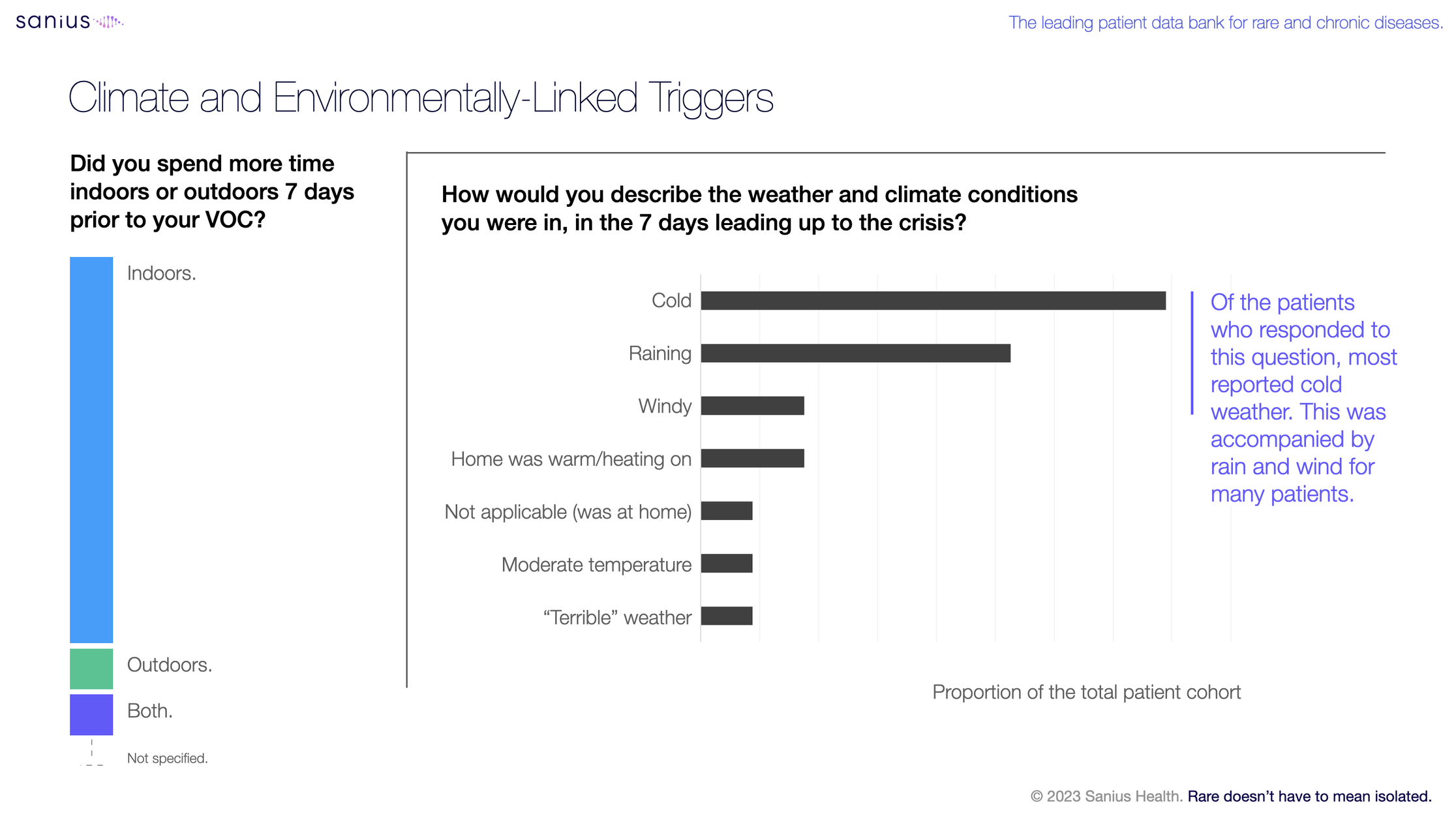
Further to this, important environmental factors were flagged in the patient responses. Despite many patients spending the majority of their time indoors in the lead-up to their VOC, weather conditions, exposure, and changes in temperature were frequently mentioned as contributing factors in the 7 days prior. Indeed, of the patients who responded to this question, almost three-quarters reported cold weather in the 7 days leading up to the crisis, accompanied by rain and wind for many patients.
Managing a Crisis.
For many patients, the first step in dealing with a VOC begins at home. With ongoing issues around the quality of care and compassion received at hospitals, compounded by exacerbation of already lengthy wait times during recent strikes, seeking clinical treatment is often the last resort. Unfortunately, this is not always possible, with most patients reporting that attempts to find positions that alleviate the pain were unsuccessful during the VOC. Over-the-counter medications such as paracetamol and ibuprofen were core parts of tackling their pain in the first instance, with morphine and codeine comprising similarly common methods of treatment during more severe crises.
For patients who ultimately seek hospital care, almost a quarter reported either having no clinical protocol, being unaware of having one, or being unsure of what it entailed. Alongside more than one third of patients who received in-hospital care during their crisis reporting either mixed or completely negative experiences, the large proportion of patients who did not go to hospital at all during their latest crisis may not be surprising. Ultimately, much like management in a home setting, patients’ clinical protocols focused on administering pain relief, as well as hydration/fluids.

Developing Insights to Drive Better Quality of Life and Outcomes.
Our ongoing work in SCD has seen a particular focus in working with patients, clinicians, and life science partners to accelerate what is known about VOCs and the changes to patient physiological and psychological wellbeing over the period that proceeds them. In deriving new learnings from patient experiences, our goal is to ultimately integrate this insight both into the wider knowledge pool to support patients and their clinical teams to improve disease management, as well as into our own ongoing work to develop predictive algorithms that prompt earlier, preventative treatment. With a growing wealth of real-world data and evidence both from patient surveys and through Sanius’s ecosystem of live PRO and wearable insights, our hope is that we are now closer to this than ever.
Already, we have seen that 78% of patients who onboard with Sanius report an improved quality of life score – a key driver in why new patients continue to join the ecosystem each day. As we continue to accelerate the insights that facilitate predictive and pre-emptive intervention, as well as education around methods of VOC management identified within the SCD community, we welcome anyone who wishes to learn more about our work in supporting improved patient quality of life to contact us at info@saniushealth.com.
The patient experience shared.
Join the Sanius Health Community
Register your interest below and a member of our team will follow up with you soon.